Athletes & Veins
You tie on your running s hoes and put in your earbuds, ready for a heart rate-raising run, but you call it quits early because your legs start to ache, or you become so tired it feels like you can't take another step. Maybe you had a great Zumba workout but thirty minutes later your legs are throbbing so badly that only elevating them brings relief.
Many athletes, professionals and amateurs alike, experience some kind of leg pain at one time or another, whether from the mechanics of pounding movement on a hard surface, or keeping their legs in the same position for extended periods. But rarely do they attribute the discomfort to a dysfunction in their venous (veins) system.
According to Dr. Todd Hansen, vein specialist and co-founder of Carolina Vein Associates in North Carolina, not all aching legs are simply due to physical activity, or even the effects of aging.
"You can talk yourself into minimizing those symptoms and not realize that it's actually vein disease that's causing them, not that five-mile run," said Dr. Hansen. "Let's change the first reaction and realize that leg pain in general is not normal, then let's investigate what things could possibly produce those symptoms."
The role veins play
While the arterial side of the human cardiovascular system has been studied extensively, much less research has been conducted on veins, also referred to as the venous system. Yet, the veins contain approximately 70 percent of the body's total blood volume when a person is at rest.
Healthy veins carry deoxygenated blood back up to the heart, while the "muscle pump" action caused by the flexing of our feet and calves help the blood to travel against gravity. In leg veins, there are valves that open to allow the blood to flow one way: up. If the valves in the veins become damaged, some blood will flow backwards into the legs and "pool" there, resulting in a feeling of heaviness, leg pain, or other symptoms. This is sometimes referred to as "venous reflux."
Who's at risk?
Some of the symptoms of vein disease are obvious: visible blue- or purple-colored "spider veins," bulging varicose veins, or even open wounds (leg ulcers) on the leg or ankle. Other symptoms are much more subtle. In addition to achiness and swelling, sensations like an itching or tingling in the legs may be an indication of vein insufficiency. Leg cramps after long periods of inactivity, or while lying in bed at night, are another possible symptom.
Some people may experience no symptoms at all, and some merely accept them as an unavoidable byproduct of physical fitness.
"You can be in great shape and still have a vein disease that's slowly developing," explained Dr. Hansen. "It's so easy to assume that your legs are tired because of physical activity. That's why primary care physicians—and patients themselves—need to be aware of the symptoms and risk factors."
Since venous disease has a strong genetic component, one of the biggest risk factors for vein disease is heredity. If someone in your family has experienced vein disorders or has visible varicose veins on their leg, your risk of the disease is much higher. If one parent has vein disease, you have a 30-40% chance of developing vein problems; if both of your parents do, your risk goes up to 80-90%.
Another risk factor is age. As the body ages, a decrease in the production of collagen causes the veins to change and the valves more likely to fail, especially in the superficial veins (veins that are close to the surface of the body), which is why there is a higher incidence of varicose veins in the elderly population. (It's worth noting that although seniors have a fifty percent greater chance of suffering from venous insufficiency, their success rates after venous treatment are no different from the their younger peers.)
Gender also plays a role in varicose veins and other vein issues. Women are almost 2½ times more likely to have vein disease than men. A woman has three "high risk" times in her life that can produce dramatic hormonal changes that influence vein health. First, menarchy; second, if she becomes pregnant; finally, when she enters menopause.
Although there are some risk factors we cannot control, there are environmental factors that can be minimized. Standing or sitting for long periods of time, especially with your legs bent or crossed, may raise your risk for vein problems. Likewise, lying in one position for too long can cause serious vein problems. Patients in the hospital or on bed rest, for example, may experience a slowdown in blood flow that can lead to blood pooling in the extremities.
How exercise impacts veins (and vice versa)
During exercise your muscles require more oxygen, so veins dilate to increase the volume of blood flowing through the circulatory system—but if your veins are not working properly, that means more blood can pool in your legs. On the other hand, exercise is beneficial from a venous standpoint because anything that improves the function of the foot and calf muscle pumps to get the blood back up to the heart is good. Most vein specialists agree that walking is the best exercise for improving the muscle-pump function, especially following vein treatment.
Dr. Hansen believes that walking is great "wherever you are on the venous spectrum," though he stresses that while walking can help manage the symptoms, it does not prevent vein problems.
Neither does exercise cause vein problems, except in extreme cases. Physical activities that require your legs to support heavier weight over prolonged periods of time, such as weightlifting or backpacking can put someone at increased risk for developing venous issues. Repeated exposure to increased intra-abdominal pressure, or pressure that is transmitted to lower extremities, can cause the normal system of valves and veins to weaken over time and become incompetent.
Repetitive motion sports such as endurance running, cycling and tennis can also put a lot of stress on your leg veins and over time may overcome a normal venous system.
In general, exercise (and working out the muscle pumps) is not detrimental for the vast majority of athletes who are participating in a more typical spectrum of activity. In fact, maximizing the efficiency of that system is beneficial.
Depending on each individual's degree of vein disease, he or she may become more symptomatic because the foot pump no longer counters the vein insufficiency. One person's level of activity, for instance, may be associated with the progression of vein disease if they have some pre-existing risk factors, such as age or family history.
While exercise can influence vein dysfunction, it doesn't necessarily prevent it or cause it. But can poorly performing veins affect athletic performance? The short answer is yes. If the venous system is not working correctly, then the "extra" de-oxygenated blood (and blood waste products like lactate) can cause discomfort, cramping, fatigue, or other conditions that diminish performance. Even if legs feel great during training, vein issues can also cause legs to hurt after exertion and slow your recovery.
Fixing the problem
If vein problems keep someone from doing activities that aggravate his or her vein symptoms, then choosing alternate activities is one way to cope. Some people may find that swimming, for example, does not produce the same discomfort that running does.
Athletes can live with the problem, but Dr. Hansen emphasizes that they don't have to: "There are so many options for treatment so that people can continue doing their favorite sports or whatever activity they're passionate about. They might even see an improvement in their performance."
Modern treatments have excellent initial and long-term success rates when performed by an experienced phlebologist (vein specialist). Endovenous approaches are minimally invasive treatments used to address specific large varicose veins in the legs. Endovenous ablation (EVLA) is considered the gold standard in the treatment of venous symptoms, with success rates between 90% and 98% after five years. It has largely replaced previous, more invasive standards of care, such as vein stripping.
Another option for treatment is sclerotherapy, performed either with ultrasound-guidance or with a light-assist, which seals the vein wall of small varicose veins allowing them to fade away.
With both EVLA and sclerotherapy, patients can walk the day of the procedure and return to normal activity, including moderate exercise, within a few days.
The key to safe, effective vein treatment is to consult with a board certified vein specialist who can evaluate the entire venous system so that poorly functioning veins can be treated at the source.
"Athletes can have vein disease with or without visible signs, so we need to be vigilant about not automatically attributing leg pain to the effects of aging or exercise," said Dr. Hansen. "There may be underlying reasons that you've never even considered."
RESOURCES
"All Men Are Olympic Hopefuls: Compression Wear Helps" VEIN Magazine. Spring 2015: 48-51.
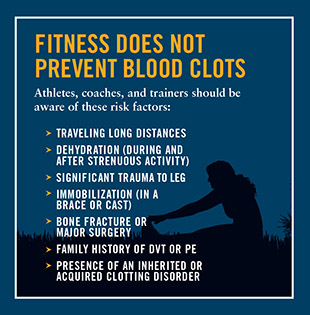
National Blood Clot Alliance. Athletes and Blood Clots. http://www.stoptheclot.org/news/article126.htm
"Blood Clots and the Athletes: A Review of Deep Vein Thrombosis in Sports" Athletic Therapy Today July 2007: 2-4.
Beliard S, Chauveau M, T, Cros F, Ecarnot F, Becker F. Compression Garments and Exercise: No Influence of Pressure Applied. J Sports Sci Med. 2015 Mar; 14(1): 75–83.
Hill J, Howatson G, van Someren K, Leeder J, Pedlar C. Compression garments and recovery from exercise-induced muscle damage: a meta-analysis. Br J Sports Med. doi:10.1136/bjsports-2013-092456
Hull C, Harris J. Venous Thromboembolism and Marathon Athletes. Circulation. 2013;128:469-471
Grabowski G, Whiteside WK, Kanwisher M. Venous thrombosis in athletes. Am Acad Orthop Surg. 2013:21(2):108-117.
This article was featured in Vein Health News, a publication founded by Dr. Cindy Asbjornsen to educate medical professionals and patients about vein health.
Dr. Asbjornsen is the Editorial Director for Vein Health News, Maine's vein magazine for primary care physicians. Read the Latest Issue and Subscribe to Vein Health News.
![]() Do I have Venous Disease?
Do I have Venous Disease?
Millions of people across the United States experience its symptoms. Find out more by asking yourself these 12 questions.
 Request an Appointment
Request an Appointment
Ready to take the next step towards understanding your vein health and the available treatment options? Click here to request an appointment.